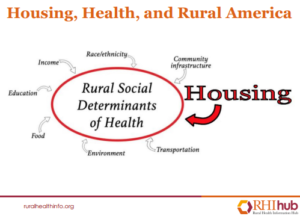
Housing and Rural Health
A review study of housing and rural health in rural America
Reproduced from:
Health in Rural America | NIH News in Health
About 20% of Americans live in rural parts of the country. Rural areas have more space, fewer people, and scenic landscapes.
Residents often have a common sense of community, but living in a rural area can also bring challenges for staying healthy. Housing and rural health are highly co-related.
Studies have found that rural Americans are more likely to die prematurely from the leading causes of death in the U.S. These include heart disease, cancer, lung disease, and stroke.
They have higher rates of obesity and diabetes. And they’re at greater risk of fatal car crashes, suicide, and drug overdoses, thus causing housing and rural health issues.
Experts are studying why some health problems are more common in rural areas. They’re also looking at ways to help.
How does where you live affect your health? The answer is complicated. Different places have different resources.
Access to housing, education, jobs, health care, and healthy foods varies across America. And all can impact your health.
“Poverty, unemployment, low education, and inadequate transportation are all known to contribute to poorer health,” says Dr. Brian Rivers, a cancer care expert at Morehouse School of Medicine.
These factors are often found at higher rates in rural communities.
Many rural communities are geographically isolated. Fewer people and more space can mean fewer local businesses and services.
That can make it harder to get the things you need to stay healthy.
Many rural Americans, for example, live far from grocery stores. Convenience stores may be the only nearby option.
These stores tend to carry fewer fresh foods, like fruits and vegetables, and more processed, packaged foods. Processed foods are usually high in salt, sugar, and fat.
Studies suggest that eating too much of them can lead to health problems such as heart disease, diabetes, and obesity.
Rural residents can also face more barriers to getting physical activity. Roads may not have sidewalks. This makes it more difficult to safely exercise. Rural areas may also lack parks for recreational activity.
“In many rural settings, folks don’t have access to fitness centres,” adds Dr. Suzanne Judd, who studies heart disease in rural communities at the University of Alabama at Birmingham.
Not getting enough physical activity can put you at higher risk for cancer, obesity, and heart disease.
Rural areas also tend to have more older adults. Older adults experience more chronic health issues than younger people. But rural residents may live far from hospitals and be less likely to have health insurance.
Another major obstacle can be finding a doctor. In many rural communities, there is a shortage of doctors.
“It’s more difficult to provide many types of health care services in rural communities simply because there’s a lower availability of health care professionals,” says Dr. Ty Borders, an expert on rural health at the University of Kentucky.
This can make it hard to get specialty care for things like cancer or drug addiction, Borders explains. Many people must travel a long way to reach a specialist or hospital. And those providers may not have the latest health technology.
“In rural communities, folks don’t necessarily have access to state-of-the-art equipment—the CT scanners, MRIs—that you might need to diagnose certain things,” Judd says. “These are particularly important when we’re talking about brain health and stroke.”
And finding a doctor is getting harder in some rural areas. “An increasing number of health systems in rural areas are closing their doors, mostly because of funding,” says Rivers. That means people may be forced to drive hours for health care.
The Role of Telehealth
Considering housing and rural health issues, telehealth plays an important role, virtual visits may be one option for rural patients.
Telehealth—delivering care on the phone or computer—has been expanding in recent years.
Physicians can monitor patients with chronic conditions without the need for them to come into the office.
This is critical for certain health conditions where providers are scarce. Someone with diabetes, for example, can take a blood sugar reading during a virtual visit with their doctor.
Patients with depression and other mental health conditions can get online counseling.
“Telehealth may be preferable for many patients and may make treatment easier,” Borders says.
Borders is studying how telehealth can be used to deliver treatment for opioid use disorder in rural communities. Most rural counties don’t have medical professionals who specialize in treating addiction.
The rates of drug overdose deaths are rising in rural areas and are now greater than in urban communities.
But telehealth can’t address every health issue. Some things require an in-person visit. And some rural areas have limited broadband service.
Also read: Incremental Housing and Design for low-Cost Housing in USA

